Major milestone reached as first-ever cellular therapy for solid tumours approved for the treatment of advanced melanoma.
The approval by the U.S. Food and Drug Administration (FDA) could mark the beginning for solid-tumour cellular immunotherapy – a field which has the potential to transform the way cancers are treated.
Thanks to the contribution of patients and researchers at The Royal Marsden, the U.S. Food and Drug Administration (FDA) has recently given accelerated approval to the first cellular therapy for the treatment of advanced melanoma. This is the first treatment of its kind to be approved for solid tumours.
The newly approved treatment, called Lifileucel, is a type of T-cell immunotherapy known as TIL therapy which involves harnessing the patient’s own immune system to fight cancer. Until now, T-cell immunotherapies have only been used to treat patients with blood cancer. Treating solid tumours with T-cell therapy is much more challenging, since the surfaces of solid cancer cells are incredibly diverse. This makes it difficult for T-cells to recognise and target them. However, thanks to research supported by The Royal Marsden and patients taking part in the C-144-01 clinical trial, this groundbreaking treatment has been shown to be effective in the treatment of advanced melanoma.

What is Melanoma?
Melanoma is a type of skin cancer which can be difficult to treat. It has a high risk of spreading to other areas of the body, becoming advanced. This is also known as metastatic melanoma or stage 4 melanoma. It can also become resistant to treatment, including other immunotherapy treatments. Thanks to another study led by The Royal Marsden, we now know that melanoma can alter its genome to hide from the immune system, resist treatments, and spread around the body.
New hope for melanoma patients who have run out of options
The FDA’s approval is based on the positive results from the C-144-01 clinical trial, a global study involving multiple cancer centres including The Royal Marsden. The C-144-01 trial at The Royal Marsden was led by Dr Andrew Furness, Consultant Medical Oncologist and Solid Tumour Cellular Therapy Lead, who is part funded by The Royal Marsden Cancer Charity.
The trial explored the use of TIL therapy to treat patients with advanced melanoma whose cancer had not responded to other previous treatments. The study found that, of 153 patients from across Europe and the U.S., more than a third of patients responded well to this innovative type of cellular therapy.

“The approval of a first solid tumour cellular therapy represents a possible turning point in the management of solid tumours” says Dr Andrew Furness.
“While current forms of immunotherapy have revolutionised the treatment of cancer in recent years, overall, these benefit a minority rather than majority of patients. This study demonstrates that even when other immunotherapies therapies have failed, the immune system can be harnessed in a different way to reliably control a patient’s cancer.”
Professor James Larkin, Consultant Medical Oncologist at The Royal Marsden was also involved in the clinical trial and a key member of the international research collaboration. He has previously spoken on the results of the C-144-01 trial, saying:
“These results show that TIL therapy could offer sustained benefits to some patients with advanced melanoma that can improve over time, which could provide a new treatment for people who currently have no other options. Along with potentially extending patient’s lives, this one-off treatment also means less time in hospital compared to treatment with other immunotherapies.”
What is TIL therapy and how does it work?
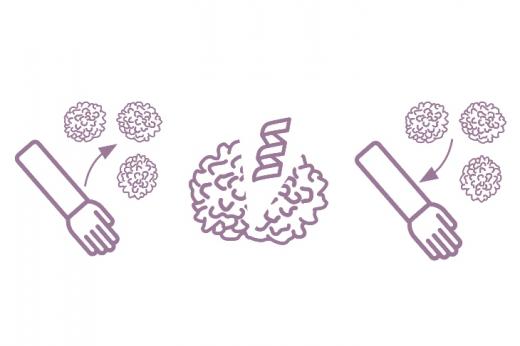
TIL therapy is a type of cancer treatment which uses T-cells from the patient’s own immune system to attack cancer cells. T-cells are a type of lymphocyte (white blood cell) which are part of the immune system and usually help the body fight off infections. While they can help the body fight diseases such as cancer, they can struggle to differentiate between healthy cells and cancer cells. As cancers grow, some T-cells recognise these cells as abnormal and infiltrate the tumour - these are the tumour-infiltrating lymphocytes, or TILs.
During TIL therapy, part of the tumour is surgically removed in order to harvest T cells that are naturally capable of infiltrating the cancer. These are then activated and expanded (grown in large numbers) in a lab before being reinfused into the patient. This gives the patient more T-cells that are better able to recognise and attack cancer cells.
Hopes for the future of TIL therapy treatment for solid tumour cancers.
“We’re continuing our research into the use of TIL therapy, as well as other forms of cellular therapy, across a broader spectrum of cancers.” says Dr Andrew Furness. “This includes advanced lung, liver, ovary, skin and testicular cancers as well as soft tissue sarcoma.”
While TIL therapy is not yet approved for melanoma treatment in the UK, Dr Andrew Furness explains, a regulatory review on the therapy will now take place in Europe and the UK. This also paves the way for earlier use of TIL therapy in a patient’s treatment journey, which will be an important focus of research over the next few years.
Your support helps fund innovative research like this.
Solid tumour cellular therapy research at The Royal Marsden is funded by supporters of The Royal Marsden Cancer Charity including a generous donation from Nationwide Building Society, and The National Institute for Health and Care Research (NIHR) Biomedical Research Centre at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London.
Thanks to your support, The Royal Marsden Cancer Charity has funded solid tumour cellular therapy work at The Royal Marsden since 2017 and part-funded Dr Andrew Furness since 2019. Find out more in our latest impact report here.
Thanks to your support we can continue funding ground-breaking research and pioneering clinical trials like this.
Want to stay up to date?
Get the latest news and stories to your inbox.


