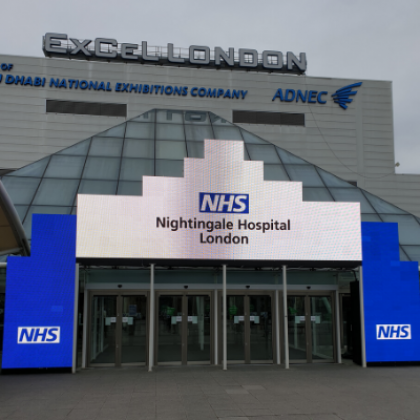
Working in the Nightingale Hospital – a first hand perspective
Dr Richard Lee, Consultant Physician in Respiratory Medicine at The Royal Marsden, tells his story of being involved in this unique experience and how lessons learned can benefit cancer patients.

Royal Marsden staff at the Nightingale Hospital
When the COVID-19 pandemic arrived, it was surreal, and almost not possible to believe it was happening. Many of the research team clinicians began working remotely or were redeployed to acute clinical areas. As a Consultant Respiratory Physician, trained in diagnosing and treating lung conditions beyond cancer, I felt compelled to support the COVID-19 response, particularly in a dedicated COVID-19 facility.
At this time, a team led by The Royal Marsden’s Chief Nurse, Eamonn Sullivan, was released from the Trust to support the leadership of the creation of the NHS Nightingale Hospital at the Excel Centre, London. Along with Chief Pharmacist Jatinder Harchowal, Clinical Assessment Unit Matron Louise Davison and Deputy Critical Care Unit Matron Deborah Scott, I was seconded as Clinical Lead for the ‘Step-Down’, or recovery team.

The initial days were about as intense as anything I’ve faced in 20 years of my career. Within a fortnight we established the standard clinical protocols that would typically evolve over years in most hospitals. Drawing on our expertise for processes already established at The Royal Marsden, we effectively designed a new hospital from scratch. My team was responsible for what would happen to patients who were ‘stepped-down’ from the Intensive Care Unit. We were asked to prepare for the imminent arrival of hundreds, if not thousands of COVID-19 patients, should the same levels of infection be seen in the UK as had overwhelmed ICUs in Italy and Spain.
We had to find hundreds of volunteer staff, fit out wards and prepare for various simulations of routine and emergency scenarios all in a matter of days. All of this was done in a ‘socially distanced’ workplace, a concept which had never existed before. We conducted meetings sat two metres apart, surrounded by fatigue-clad military staff. The ‘Nightingale way’ defined a completely new approach to leadership and healthcare that reflected on its processes in an hourly, rather than monthly fashion and embodied a flat hierarchy with daily clinical management briefings where every voice counted. A bona fide ‘learning hospital’.
The Nightingale's first patients
As the first patients arrived, planning became deployment. Our first moments on the ward were daunting but the tasks were well matched to our clinical roles. I’ve spent thousands of hours on call, managing respiratory failure, critically ill patients, and have been responsible for triaging large volumes of medical admissions in teaching hospitals, yet this was an entirely different experience - ‘donned’ from head-to-toe in tightly fitted, constrictive PPE, which made conversations at anything other than arms reach near impossible and merely breathing felt like an overly prolonged visit to a steam room. We trained in hand gestures to command simple urgent instructions and electronic patient noting systems.
In the end, we were very fortunate that the facility did not reach anywhere near its capacity. It excelled as a busy ICU whilst beds across London also took up the strain in more appropriately resourced hospitals. Londoners, with the NHS in their hearts and minds, clapped us home from work each Thursday evening, embraced social distancing with a considerable respect to protecting both each other, and our NHS staff.
As patient numbers reached a plateau and we could transfer patients out, the difficult decision was taken to de-escalate Nightingale and package it up ready in case of future need. Lessons learned have been documented, effectively serving as a ‘pandemic preparation plan’, a recipe book for what we will do if faced with the worst again.
No doubt we will look back and be hugely grateful that we had been able to prepare so rapidly to be ready for whatever the worst might have been. We might still face a second spike, hopefully manageable with our growing and collective efforts at infection control as a nation.
In medicine we are comfortable with dealing with the unexpected, tackling challenges head on, and quickly, professionally and effectively working with new groups of colleagues. The entire Nightingale team was made of some of the strongest, brightest and most committed clinicians and support staff that I have seen, brought together so rapidly. All worked tirelessly, courteously and with conviction to be ready, no matter what. Some resided on site, not seeing their families for weeks.
Being part of Team Marsden
The presence of ‘Team Marsden’ alongside me was invaluable in what might otherwise have been a lonely experience. Knowing that our experts were at the helm was incredibly reassuring as we planned for the unknown. The friendly, informality of being sat down by The Royal Marsden’s Chief Nurse, for a coffee, at the start of one shift, just to check-in, offer advice, check that we were doing ok, just because that was the normal way to work, was deeply comforting.
Bringing The Royal Marsden way to the Nightingale, in a different setting was a privilege, with the feeling of being in the same ship, in stormy weather amidst a great team.
Landing back at The Royal Marsden, we have drawn parallels and thought about how we will work differently and more innovatively than ever. New working patterns have meant that I have been able to teach my children for a few hours in the morning before heading to work on a deserted train, or to my ‘bedroom office’ using video-conferencing technology with patients and fellow researchers. I’m sure that the lessons learnt, in what was essentially a field hospital in an enormous warehouse, on the opposite side of London will benefit Royal Marsden cancer patients in the least expected ways for years to come.
Returning to The Royal Marsden
We are now striving hard to bring things back to a new, better, normal for our cancer patients, at The Royal Marsden. Since returning, I have set up a research study funded by The Royal Marsden Cancer Charity that will use artificial intelligence to understand how COVID-19 can mimic cancer therapy toxicity to help clinicians to rapidly differentiate between the two, and define the most appropriate treatment.
Furthermore, at a time when we’ve seen the greatest fall-off in patients coming through the NHS for new cancer diagnoses than I have ever seen in my career, early diagnosis will be more important than ever. We are creating new patient pathways using ‘COVID-clean’ or ‘green’ facilities, that are safe for our non-coronavirus affected patients. Finding new ways to identify early stage cancers that can be treated effectively, whilst minimising the risks to cancer patients who may otherwise be considered vulnerable will be absolutely essential to improving cancer outcomes in the post-COVID era and The Royal Marsden Cancer Charity have been hugely supportive in our ambitions to do so.
The last few months have been challenging for all of us; clinicians, other healthcare professionals and most importantly, our patients. Such uncertain times will push us to excel in new ways and The Royal Marsden supported by The Royal Marsden Cancer Charity will not be shy to take the best of these new ways of working forward as the new ‘Marsden way’, of tomorrow.



